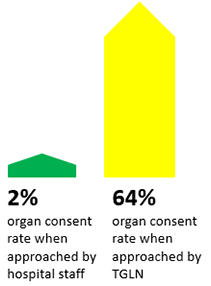
Kidney and Pancreas
ADULT
Liver and Intestine
REFERRAL & LISTING CRITERIA
Liver
ADULT
PAEDIATRIC
Intestine
ADULT
PAEDIATRIC
FORMS AND HANDBOOKS
Liver Transplant Referral Form
Liver and Liver/Bowel Special Case Committee (SCC) Exception Application Form
Clinical Handbook for Liver Transplantation
FAQs: Clinical Handbook for Liver Transplantation
Colorectal Liver Metastases Transplant Exception Application Form
Lung
REFERRAL & LISTING CRITERIA
ADULT
PAEDIATRIC
Heart
REFERRAL & LISTING CRITERIA
ADULT
PAEDIATRIC
FORMS AND HANDBOOKS
Heart Special Case Committee Exceptions Application Form
Clinical Handbook for Heart Transplantation
FAQs: Clinical Handbook for Heart Transplantation
Ontario Clinical Guidelines Ventricular Assist Devices
Addendum - Ontario Clinical Guidelines - Ventricular Assist Devices for Destination Therapy
Advanced Heart Failure Therapies Referral Form
Considering a Left Ventricular Assist Device - Guide for Patients and Caregivers
Tissue